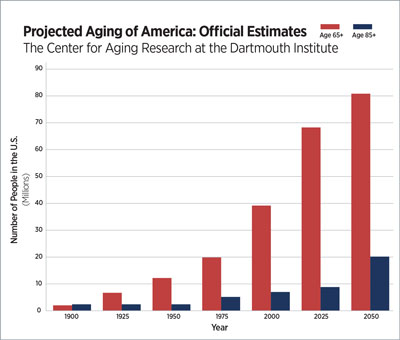
Between 2011 and 2031, the number of adults age 65 and older is expected to double, and those 85-plus will increase fivefold. An aging population reflects improvements in healthcare and wellness that have led to longer life spans, but it also means growing numbers of Americans will require more services for an increasingly complex set of health needs.
Facilities that serve aging Americans, either in acute care or long-term care settings, will not just be staying busy. They’ll also need new strategies and techniques to recruit and train their staff to meet the changing needs of a more active, engaged and digitally savvy population of older adults.
Changing Healthcare Demands
The needs and expectations of today’s older Americans are quite unlike those of the seniors who have come before them. For instance, rather than drastically slowing down their lives by age 65, today’s seniors have a longer life expectancy and largely choose to remain active.
“When I was a child, older people were cared for at home or went into a nursing home,” says Darrel Weatherford, vice president of AdvantageTrust, the HealthTrust division for non-acute facilities. “What used to be considered old is not old anymore. People are working and living active lives into their 70s and 80s. They want choices, and that has caused the senior housing and care industries to dramatically expand the options available to seniors over the past
10 years.” This has included development of high-end senior living facilities and communities, many of which include a wealth of activities and opportunities both on-site and off-site.
As baby boomers age, their expectations for healthcare will become even more robust, says Nash. “They will want a certain level of connectivity with their providers,” he says. “We will be seeing technology to help people stay at home and age in place. We’ll also need better information technology to enable constant communication with doctors, nurses, pharmacists and other healthcare professionals. I think we’ll see ways for healthcare providers to remotely regulate and check patients’ urine, temperature and even emotions.”
Patients won’t just be interested in communicating with their healthcare providers; they’ll also be interested in communicating about healthcare providers.
Another significant trend will be public transparency related to healthcare, Nash says. “We’ll see unprecedented levels of accountability. There will be physician-specific [performance] measurements available online, and patient evaluation tools just like Yelp [an app that collects crowdsourced reviews about local businesses].”
In addition to the demands for ongoing communication with healthcare providers, Nash predicts there will be an explosion of new technology to help seniors cope with clinical problems associated with their new hips, knees and corneas.
These new ranks of older adults will also be less likely to blame health declines on aging and insist on solutions. “Way too many times, older patients have been convinced by themselves or others that their pain, their difficulty getting up from a chair or their depressed feelings are untreatable parts of growing older,” says Steven Stein, M.D., chief medical officer of continuing care at Livonia, Michigan-based Trinity Health. “More often than not, while there may not be a cure, there are strategies that will lead to incremental improvement.”
Care providers could work to reduce the amount of polypharmacy (taking of multiple medications concurrently to manage coexisting health problems) among the elderly. “The number of older adults on eight or more drugs is just astounding,” Stein says. “I give you my permission now to stop my pill to reduce my cholesterol, take away my baby aspirin and get rid of all of my vitamins if, in the future, I’m still on any of these and I am in the later stages of Alzheimer’s.”
Stepping Into the Gap

HealthTrust Workforce Solutions℠ Addresses Nursing Shortage With StaRN Program
The market for qualified nurses is highly competitive—and poised to be even more so as the number of aging Americans in need of healthcare services continues to increase. Many health systems lack the time and resources to on-board and train new nursing graduates, so they often draw from a small pool of qualified nurses, all while nothing is being done to grow the pool itself.
That’s why HealthTrust Workforce Solutions℠ developed the Specialty Training Apprenticeship for Registered Nurses Program (StaRN), an innovative solution designed to address the shortage of nurses. “It is helping hospitals across the country get the increasing numbers of qualified nurses they need to deliver care to a growing patient population,” says Brendan A.J. Courtney, president and CEO, HealthTrust Workforce Solutions℠.
StaRN provides intensive post-graduate education for recent nursing graduates, including comprehensive didactic training, a robust simulation experience and a hands-on clinical preceptorship. The curriculum also emphasizes the importance of interpersonal communication and patient relations, which are critical skills needed to help aging Americans maintain autonomy in healthcare decision-making and delivery.
“Upon completion of the program, graduates are equipped with the knowledge and skill to begin their careers,” Courtney says.
For more information, visit www.parallon.com/services/workforce or contact your account director.
Preparing to Meet New Needs
If they are to meet the changing needs of aging Americans, healthcare facilities “must start paying attention and making investments in infrastructure now so they will be ready for the future,” Nash says.
Jefferson University Hospitals, for instance, is investing in private technology companies that are building new telemedicine and electronic medical records programs.
Healthcare facilities are already working to assemble the workforce that will be needed to serve growing numbers of aging patients. According to the American Society on Aging, the United States will need an additional 3.5 million healthcare workers by 2030 to maintain the current ratio of healthcare workers to the population.
“We definitely need more primary care providers, physical therapists and nurses,” says Marcia Donlon, RN, BSN, MS, administrative director of primary care/care continuity at Holy Family Memorial (HFM) in Manitowoc, Wisconsin. To fill those openings, HFM is providing extra value to potential candidates.
For instance, the hospital has established scholarship programs for nurses and other healthcare workers who want to return to school for additional training. Those working to earn a nursing or physical therapy degree can get significant scholarship dollars, and then come back to work when they complete the degree. HFM also welcomes students to participate in job shadowing programs to encourage them to enter into nursing and other careers.
“The demand for new nurses will be greater than we can meet” as baby boomers continue to retire, Donlon says. “Some of the specialty positions are particularly hard to fill. A lot of organizations offer bonuses, but I don’t think the money is as important to employees as work-life balance.”
Another option is to offer four-hour shifts to nurses who are nearing retirement age to encourage them to continue working. In other cases, it is redefining job duties to keep them working longer, such as allowing nurses to focus on bedside care and leaving technical responsibilities to others.
To help keep nurses on board, HFM also offers flexible scheduling and job sharing. “Maybe one nurse wants a month off in the winter to go to Florida and someone else wants a month off in the summer to visit a vacation home, so we try to make that work,” Donlon says.
While there is certainly a shortage of healthcare workers, not all positions are in demand. “We do not have a doctor shortage; we have a primary care doctor shortage,” Nash says. “We have a surplus of specialists and not enough primary care doctors because we don’t pay them enough.”
To help remedy the shortage, many facilities are working to convince medical students to enter the field of primary care by offering student loan forgiveness and other incentives. Another way to attract more physicians to primary care could involve cultivating a culture of teamwork among healthcare practitioners, Nash says. “Appoint doctors as team captains and empower team members to work together to meet the needs of an aging population.”
To help organizations find solutions to the scarcity of healthcare workers, the American Geriatrics Society is creating a Geriatrics Workforce Enhancement Program Coordinating Center. The center will serve as a strategic resource for 44 organizations around the country that are working on projects to increase the numbers of doctors, nurses, social workers and other professionals trained to care for older adults. Program goals include supporting geriatrics education, training diverse and interprofessional teams of healthcare providers, maximizing older adult and caregiver engagement with the healthcare system, and improving health outcomes for older adults.
Facilities need not only more healthcare workers to serve the aging, but professionals who can do so with grace.
“We need to build a workforce that supports our elders with the reverence they deserve,” Stein says. “As we age, autonomy in our decision-making and independence in our movement become things we value more than ever. Caregivers and healthcare providers need to be really good interviewers and listeners so they understand what makes life worth living for the individual.”
Stein explains that his experience as a geriatrician has demonstrated that most people age 85 and over worry more about maintaining quality of life and are less concerned about how much longer they may live. “They do not appreciate family members, friends or healthcare providers focusing on the things they no longer can do well; instead, they are happier and more fulfilled when they can successfully navigate the situation at hand.”
For instance, people with dementia may become frustrated if their memory is repeatedly tested, but may feel gratified when they can contribute with skills they have retained, such as the ability to fold laundry or read to a grandchild, Stein says.
In addition, practitioners must become more comfortable having discussions with older adults about their end-of-life wishes. “Most studies suggest that the older adult wants to talk about it but are waiting for the physician to bring it up, while the physician is waiting for the patient to bring it up,” Stein says. “Having the discussion and documenting these end-of-life care wishes may be one of our greatest opportunities.”
Developing Solutions
Many facilities are already finding ways to connect with aging adults and provide better, more targeted care for them. At Trinity Health, skilled nursing facilities and home care agencies are successfully working together to ensure high-quality, seamless transitions from setting to setting and provider to provider.
“Our home care agencies, hospices and skilled nursing facilities are leveraging telehealth services to improve access to physician services,” Stein says. “We have made the development and implementation of a standardized advance care planning process one of our top priorities for the coming year.”
AdvantageTrust Provides Contracts for Senior Care Needs
Healthcare facilities specifically targeted to serve aging adults have different purchasing needs than acute care facilities. That’s why AdvantageTrust, the HealthTrust division that deals exclusively with non-hospital members, maintains contracts for a number of products that are in demand for senior living facilities.
“Hospital stays are generally very brief, while someone may live at a long-term care facility for the rest of their life,” says Darrel Weatherford, vice president of AdvantageTrust. “Products used in these facilities often need to perform at a different level than those used in hospitals for an episodic event that lasts a few days.”
AdvantageTrust contracts cover a number of in-demand items for senior care facilities:
> Food, including high-end, restaurant-quality ingredients
> Adult incontinence products
> Medical/surgical products such as gloves, needles and syringes
> Office supplies
> Facilities management products and services such as paint, drywall, carpeting and HVAC
For more information, visit www.advantagetrustpg.com, email memberservices@advantagetrustpg.com or call (866) 841–2992.
A new telemedicine program at Holy Family Memorial, HFM Right Now, allows patients to call and respond to a series of questions about their symptoms and conditions, and a provider will call them back within an hour. If needed, the provider will tell the patient to come in for evaluation. But in many cases, care and advice can be provided by phone.
“The cost is $35, and it keeps people from having to pack up and go to the doctor when they’re feeling sick, unless the provider says they need to come in,” Donlon says. “We are seeing an increased use of this program.”
In addition, HFM partners with three local long-term care facilities, operating health clinics in all three that are open to facility residents and the public. “The residents love them,” Donlon says. “They don’t even have to go outside. They have a clinic in their own complex.” (Read more about HFM on page 41.)
HFM also focuses on keeping costs down for consumers. “People with high-deductible plans are unlikely to seek healthcare until the situation is dire,” Donlon says. “We try to take into consideration what tests are appropriate for each person. If someone has bronchitis, for instance, is a chest X-ray necessary or are there other things we can do? Do we really need to order a CT scan before trying other interventions and diagnostics? People are starting to realize that our facilities are less likely to run costly, unnecessary tests, and we will try to avoid those costs when we can.”
Finally, HFM is working to educate aging members of its population about healthcare topics through presentations to community groups and service clubs.
“We have a large population of baby boomers and beyond, and we’re really working with them to stay healthy,” Donlon says. “We offer programs like fall prevention and wellness, making them aware that what they do now can determine their longevity and quality of life later. Many baby boomers are in a sandwich generation, still caring for their own parents and maybe young adult children, and it’s hard for them to see that they belong to an aging population. But we’re trying to do community outreach and promote it as something fun. Aging can be done healthfully.”
Share Email



