The following article by Johnson & Johnson Health Care Systems team members Amy Bucher, Ph.D., Raphaela O’Day, Ph.D., Emily Benadon, Kimberly Whelan and Somi Kim was originally published in the Nov/Dec 2014 issue of CAPG Health Magazine: The Voice of Accountable Care Groups. It has been repurposed with permission.
Patient engagement is a burning issue for healthcare providers but not necessarily for patients.
The Affordable Care Act (ACA) has heightened the focus on optimizing patient outcomes, whether that means maximizing biometric outcomes or minimizing hospital readmission rates. The fact is that good care doesn’t just come from inside the health system. Many, if not most, of the factors that predict patient outcomes are patient behaviors. For the best possible outcomes, patients must be engaged in their own health.
Unfortunately, even as we recognize the growing need for an engaged patient population, research suggests that patient attitudes are moving in the wrong direction. In 2012, Deloitte published a report that found one out of three healthcare consumers self-identify as disengaged, see little need for preventive care and have low interest in health education. In fact, a lack of understanding of what is required to be healthy is associated with poor health outcomes. People who lack the skills, ability and willingness to engage in their own health may incur up to 21 percent higher healthcare costs than other people.
So, how do you get patients invested in their own health?
Johnson & Johnson Health Care Systems created a cross-functional team with representatives from behavioral psychology in our Wellness & Prevention team, our Global Strategic Design Office, our Market Research Insights and many other functional teams to address that question. Together, we leveraged behavioral science theory, market research insights and case studies of successful interventions to develop seven principles for sustained engagement that can be used to enhance any interaction a healthcare organization might have with its members.
Data supports that the engaged patient is one who takes ownership of his or her own health, and works in collaboration with providers and supporters to achieve the best possible outcomes. We have defined this network of individuals as the ecosystem or community of care. In order for patients to be actively engaged, their values, beliefs and behaviors must be taken into consider-ation, and they must be encouraged to participate, engage and help build a community of care.
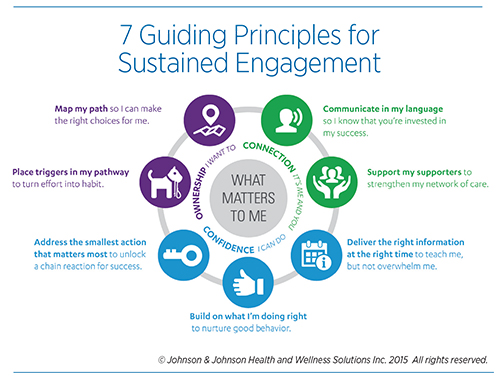
The seven principles of sustained engagement that we’ve created are organized on a framework based in motivational psychology. There is a deep body of research that shows people share fundamental psychological needs, and that a motivating experience is one that helps fulfill those needs in some way. The three most basic needs that form the hub of our framework are connection, confidence and ownership. Patients must have some sense of control over their health experience and believe in their ability to feel understood and accepted, and take action.
As our definition of sustained engagement suggests, we believe that engagement happens both within the patient and within the patient’s system of care. Many parties have critical roles to play in the collaboration that leads to improved outcomes. When all individuals within the system of care are able to use the principles of engagement effectively in interactions with patients, those patients will be more motivated to follow through on the behaviors to support their health in their daily lives.
Here are some of the ways that the community of care surrounding the patient, including the healthcare providers, can support each of the three basic psychological needs for their patients:
Connection: People who feel connected to others not only feel like part of a community or social group, they also feel recognized and understood. They can reach out to others for support in a way that advances their goals. Connection is the basic need where interpersonal dynamics between provider and patient are most critical. Strong, empathic and active listening skills can help a patient feel engaged. Using language that is meaningful to the patient and reflects back the patient’s goals is an important aspect of creating the supportive relationship. Because being able to rely on friends, family or community members while coping with a health issue is also critical to motivation and self-care, another principle urges the inclusion of supporters in patient care when possible. Offer tools, resources and information when available to the people who matter in the patient’s life, so that they can be more effective in supporting the patient’s behavior change.
Confidence: People feel a sense of confidence when they experience success. When they are not successful, they can still feel confident if they receive clear and encouraging feedback on how to improve performance. A confident and competent patient is armed with a set of skills that can be applied in a challenge, while a supportive provider stands ready to offer appropriate and helpful evaluations. The guidelines that support confidence include tailoring instructions into digestible pieces to help patients receive the right combination of skills without becoming overwhelmed, and timing feedback to arrive when the patient is able to take action. In addition, we suggest providing positive feedback—often overlooked in an environment that emphasizes correcting mistakes—and prioritizing behavior changes that will set the patient up for success.
Ownership: When people take ownership of their health, they take action not because they believe they should or have to, but because they want to. Even though many health behaviors, including modifying diets and adhering to medications, may not hold inherent appeal, when patients see them as instrumental to a personal goal, then they will develop a sense of ownership. Our engagement guidelines related to ownership emphasize understanding patients’ habits and rituals, and helping them to fit care behaviors into existing structures when possible. We also recommend as much transparency as possible around both short- and long-term expectations, so that patients feel informed about their care journey.
This framework offers a way for providers and health systems to collaborate more effectively with patients to optimize outcomes. Importantly, the principles of engagement can be applied to any touch point with the patient, including face-to-face, telephonic outreach, digital interventions, print communications and smartphone apps. These principles, when implemented appropriately and consistently, can help providers create a supportive and encouraging voice to the patient. Additionally, applying these principles within one’s own organization can build a culture that delivers on commitments in a more engaged and collaborative way. Our research suggests that implementation of the principles will inspire patients to take action in managing their own health, leading to the shared goal of enhanced outcomes.
References: Ryan, R. M. & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development and well-being. American Psychologist, 55, 68-78.
Hibbard J., Greene J., & Overton V. (2013). Patient Activation and Health Care Costs: Do More: Activated Patients Have Lower Costs? Health Affairs. 32 (2): 216-222.
Share Email





