How improving supply chain workflow for nurses can benefit health systems & patients

Today’s most effective hospital supply chain teams are those who work with end users to identify the most cost-effective supplies while maintaining quality patient care and end-user satisfaction, says Rebecca Holt, AVP, Clinical Supply Chain Solutions at Ardent Health Services. That means looking into the suppliers’ pipelines to compare availability with the hospitals’ projected needs. It also means investigating alternate products and devices, and rethinking care processes, involving the nursing staff.
This concept became exponentially more challenging during the pandemic with initial supply shortages experienced across the globe, as well as the ongoing disruptions to healthcare (and other) supply chains. Setting goals to put nurses at the center of supply chain processes can have positive trickle-down effects for nurses, health systems and patients alike. Here’s how.
Begin with understanding

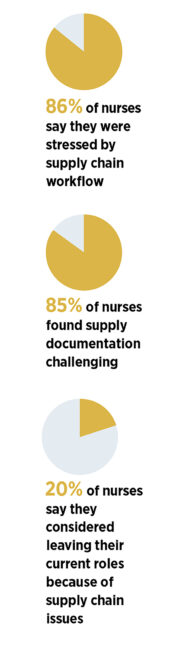
A nurse’s role is to take care of patients first. But it also requires working within the constraints of the supply chain and understanding how it works, says Suzanne Smith, RN, BSN, Solution Advisor at Lumere, a GHX company, and board member and Western Regional Director of the Association of Healthcare Value Analysis Professionals. The supply chain dilemma can be frustrating and stressful. In an industry survey of 100 hospital nurses, 86% said they were stressed by supply chain workflow, while 85% found supply documentation challenging. Issues with supply chain led approximately 20% of nurses to say they considered leaving their current roles.

While most supplies are ordered by the supply chain staff, some are managed by clinical staff, which can affect availability. Recognizing and solving this pain point can go a long way. “We started looking at where this is occurring and asking those staff members if it was something we could take over for them,” says Chris Mitchell, AVP, Supply Chain Operations, HCA Healthcare. “We determined that we could help them manage supplies to allow them to manage patients.”
Streamline procedures for gathering & tracking supplies
The process of gathering and accounting for supplies can differ by health system, facility and hospital unit. On medical/surgical floors, nurses might collect products from a supply or “point-of-use” room, selecting the patient’s name from the supply room computer and scanning the product, which links to the warehouse for replenishment purposes; other processes involve a sticker system. Not all methods are the same, and caregivers might not have enough time for training sessions and complicated processes. HCA Healthcare created 12 point-of-use supply categories in some locations to improve workflow and make it easier for nurses to find what they need.

Inconsistent or burdensome procedures can also add to staff frustration. “While it does not take significantly longer to scan a supply, the perception is that it adds additional staff time,” says Vicki Riedel, RN, BSN, Director, Clinical Resource Analysis, HCA Healthcare. When a staff member is busy or something is urgently needed, scanning may get skipped. That can put items at risk for creating a shortage (although some systems have back-end processes to mitigate that issue, Riedel adds).
Staff may also be hesitant to take time to adhere to new administrative processes because they consider patient care the top priority. “Scanning supplies for a replenishment system has been likened to scanning groceries and not really necessitating a college degree and clinical experience,” Riedel explains. However, while these steps are not directly related to care, they require clinical knowledge and can impact patient outcomes, helping avoid misused supplies and ensuring that adequate inventory is available.
While improper tracking can result in supply shortages, it can also impact hospital revenue and patient care. “Anything implanted must be scanned or manually entered into the medical record for billing,” says Holt. Items brought into a patient’s room cannot be returned to the central supply. Instead, they must be discarded or sent home with the patient, which can cost the facility money, as these items are generally not billed.
Ensuring consistent, simple and efficient processes for tracking can mitigate many of these pitfalls. Some facilities use easier scanning tools, like a weight-based bin, where the patient is charged for the supply based on the weight of the item removed. Others use a door-mounted scanner that automatically tracks supplies leaving the room. A smartphone device can also be used for scanning, eliminating the process of selecting the patient’s name from a computer screen or picking up a scanner.
Minimize the impact of supply chain disruption & shortages
 Due to the pandemic, hospitals have had to source the same products and equipment from multiple suppliers, and substitutions are common.
Due to the pandemic, hospitals have had to source the same products and equipment from multiple suppliers, and substitutions are common.
While some item substitutions, like emesis basins, may not be of consequence, bringing in alternate supplies that staff members aren’t comfortable using can put nurses and patients at risk. Safety needles are a good example, Smith says. “Every single safety needle mechanism deploys differently,” she explains. “If I don’t know how to deploy the safety mechanism, I could stick myself or hurt the patient, and no one wants that to occur.”
Unavailable items can result in a care delay, potentially impacting patient outcomes. Without the right supplies, for example, an incontinent patient could suffer skin breakdowns. “A lot of it is basic supplies,” Smith adds, though shortages of medications, oxygen, ventilators and other treatments can be life-threatening.
Communication about substituted products is also key. Changes should be shared on the intranet, via email, with cards placed on the stocking bins or shelves by the impacted supplies, or on stickers applied to the packaging. Be sure to include who to call with questions.
Traditionally, supply chain staff is not in the hospitals 24/7. So on the weekends, supply rooms should have enough supplies to cover three to five days, says Mitchell. But due to backorders, heavy utilization and shortages, that proves difficult.
HCA Healthcare evaluated its staffing models to provide flexible staffing for better coverage in some locations, including the addition of weekend hours. “Another possible response is to roll temporary carts and shelving into supply rooms when staff isn’t available, to provide the needed volume,” explains Mitchell. The temporary storage is then removed when supply chain staff returns.
Emphasize standardization
“One thing we’ve learned as an industry is the power of standardization with supplies and equipment,” says Holt. In the beginning of the pandemic, Ardent moved some staff and the majority of its ventilators to two New Jersey hospitals. The ventilators were different than the ones the staff used previously. They realized they needed to account for the learning curve for staff or nurse ramp-up time. “While they can certainly learn how to use them, it may take one or two shifts to become accustomed to that particular model,” Holt explains.
In a new facility setting, staff members may also have to work with unfamiliar beds, lab requisitions, standard order sets, IV pumps and pharmaceutical ordering. “We learned that to be able to move equipment and staff around, we have to be standardized,” Holt says. “That was a huge focus for 2021, and we’re restructuring to make it an even bigger goal in 2022.”
Ardent is consolidating to one or two suppliers for equipment like ventilators and CPAP machines. “We want to be able to take ventilators from New Mexico and send them to East Texas or New Jersey, and know that when it arrives there, the entire clinical staff will know how to use it,” Holt says.
HCA Healthcare was already starting to standardize products prior to the pandemic, partly to aggregate spending and drive down costs. “I’m not sure we’ve ever felt the pain of non-standardized supply categories more than during the pandemic response,” Mitchell adds. With 23 consolidated distribution centers, having non-standardized products and equipment makes it difficult to transfer supplies to where needs are the greatest. Using different brands for gowns and gloves is not a problem, but with equipment like ventilators, there is a low margin of error for ensuring availability.
Involve nurses in the vetting process
“I think of nursing as the core of our supply chain operations,” says Mitchell. “I value nursing feedback, which helps us understand the products and services patients need, and helps us adjust as the care landscape evolves.”
At Ardent, nurses and other staff members can suggest new products or technologies for their units through a value analysis team (VAT), explains Holt. The staff member shares the item’s value to patients or staff, how it affects patient care, impacts cost, and the potential impact on patient satisfaction and quality. The VAT also considers whether a similar item is already in use within the organization.
When replacing a product or device, the VAT calculates need and ensures the distributor has enough supply. “There’s nothing worse than changing out a product and discovering you can’t get that product,” Holt explains. Then, the current stock must be taken off the shelf and is sometimes sequestered to one unit. End users may receive product education from the supplier. “It’s a lengthy process, but it involves the key decision-makers,” Holt adds.
It’s important to have a multidisciplinary group vetting new technology at the ground level, agrees Smith. When selecting suppliers, end users should be part of that process to ensure that their questions are answered and all stakeholder needs are met. “That way, you get buy-in right away,” she says. “Not including key stakeholders can result in automatic resistance.”
Read more about HealthTrust’s supply disruption efforts.
Share Email Nursing, Operations, Q2 2022




