Moving to Practice-based Purchasing
To move toward mature value analysis, a hospital or health system must understand all costs associated with caring for individuals and communities, deliver quality care aimed at achieving the best possible health, and achieve financial results driven by exceptional patient outcomes. A highly functioning value analysis program ensures financial efficiency and optimal patient outcomes through clinical efficacy.
Resources, tools and techniques are necessary to achieve maturity in value analysis.
A value analysis toolkit should support the following five key processes:
1. Assessment

“The first step in any continuous improvement process is knowing where you currently stand,” says Vicki Alberto, vice president, clinical resource management at HealthTrust. “When you want to shift your purchasing focus to the patient, you need an objective view of which maturity level your hospital or IDN is on.”
To accomplish this, Alberto recommends using a value analysis maturity tool to assess the current program. This assessment can be done by holding departmental or individual meetings with C-suite leaders, supply chain leaders, clinical leaders and key stakeholders who are actually using the products. During these sessions, team members should be asked to comment on what’s working best and which areas can be improved and be made more efficient.
“Key stakeholders’ perceptions will differ, but there are no wrong answers,” she says.
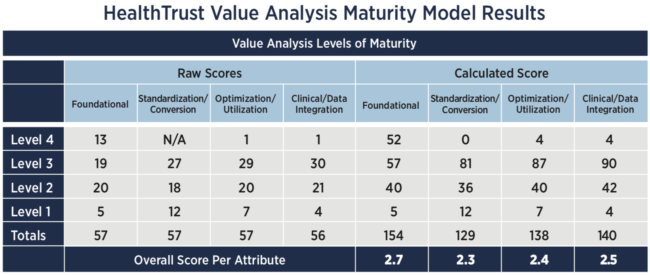
The value analysis maturity model shows these varying perceptions objectively using a scoring system. “It’s important to present the responses as numbers, so they’re there in black and white,” she explains. The team inputs raw responses to the tool, tallies them and calculates averages to assign a value analysis level based on overall response. (See Table 1.)
In addition to the surveys, Alberto’s team asks each stakeholder a series of questions that will later be part of the verbatim responses shared with leadership. The questions point to certain levels of the value analysis tool such as poor communication, but they also offer potential solutions. If the hospitals across a health system are using different devices, there may be variability in the level of care.
The value analysis maturity model offers guidance on key attributes and how to reach the next level.
2. Information
“At every phase of a value analysis process, good data is key,” Alberto says. “Through evaluating capabilities and resources, you inform product or service selection, ensure compliance and identify waste.”
Data analysis tools should include:
- Opportunity Assessment – A deep dive of clinical and financial data, as well as external market data, can help you understand your hospital’s dynamics, determine product utilization and variation, pinpoint places to eliminate redundancy and validate potential savings up front.
- Clinical Review – Review of published clinical evidence and industry observations is an exercise that should happen by each service line. “While the categories and levels of evidence may be difficult to interpret,” Alberto explains, “as you add physicians to the value analysis team you bring clinical experience and scientific method to data analysis.”
- Benchmarking – Benchmarking can help you identify clinical variation from best practices, deliver procedural and product-specific insights, and inform pricing decisions.
- Reporting – Hospital clinical and financial data should be combined to create online reports or interactive dashboards that illustrate clinical compliance and cost per case. Insights are shared with physicians and decision-makers at the hospital level.
3. Organization
“The value analysis team should strive to achieve Level 4, a clinically influenced, evidence-based culture across the continuum of care,” Alberto says. “In order to accomplish this, it’s important to establish the processes that will give your value analysis program a strong foundation.”
Key tools that support a dynamic value analysis process include:
- Value Analysis Charter – A written document that outlines how the process will work, including committee structure, data review and compliance monitoring.
- Multidisciplinary Committee – An enterprisewide committee structure that includes top-down support and engaged physicians, nurses and other stakeholders to sustain the initiative.
- Standard Agenda – A format for every meeting that ensures team members are prepared when they come to the table.
- Products/Services Evaluation – A process to generate discussion, build consensus and, when appropriate, motivate change around clinical preference items. Team members will be assigned accountabilities, and leaders will monitor key metrics.
According to Alberto, “If you’re a stand-alone hospital, you have one value analysis team with representation from all the key departments—supply chain, surgery, nursing, finance and cath lab. If you’re a health system with more than one hospital, it may be beneficial to form teams by service lines with a financial representative to help guide and answer questions specific to reimbursement.”
4. Communication
Because value analysis is a collaborative effort among leadership, clinical teams and other key players in the organization, it is important to communicate the process across departments and build confidence with early wins. “People do receive messages differently,” Alberto says. Corporate leadership might think it has sufficiently communicated a decision through its departments by simply sending an email or scheduling a meeting, while staff might claim to never have heard about the initiative.
“If departments report that they’re not getting feedback, it’s taking too long or leadership is not responding to their needs, you won’t get any participation in the future,” she continues.
A communications plan can help lower staff frustration and ensure a high level of supply chain/clinician engagement. The written plan should incorporate strategies for:
- Leadership Engagement – Messages aimed directly at the C-suite and other high-level leadership to help them understand the hospital’s unique operating environment.
- Physician Engagement – Strategies to build relationships between hospital administration and physician leaders. “As you integrate physicians into the evaluation process,” Alberto says, “it’s critical to get their commitment—some are more ‘in’ than others.”
- Organizational Alignment – Effectively communicating the rationale for product standardization and services selection is key. On scheduled conversions, the plan should outline which hospital departments will evaluate the product and then develop a plan that includes education, if needed, and conversion assistance.
- Operational Alignment – The supply chain team needs to be in tune to the pending changes. They are responsible for all the logistics required to bring about an effective conversion and have the appropriate product available—the right product, through the right route, in the right place, at the right time. This includes efficient utilization of current stock as well as initial inventory of the new products.
- Vendor Alignment – Effective communication to the supplier and/or manufacturer communities is critical to determine timelines for education and in-service, as well as provide business partners time to adjust inventories or ramp up manufacturing. Plans should include facility contact names and appropriate times they can be contacted by field representatives.
5. Optimization
A full value analysis maturity program requires top-down support, a clinical evidence review process and physician engagement. The value analysis committee has the means and resolve to examine spend data in the context of best practices.
Internal utilization requires analysis tools that help you:
- Understand the impact of various payment policies on reimbursement.
- Anticipate and swiftly respond to disruptions in the supply chain—such as a drug shortage—so patient care is not compromised.
- Understand the impact of all medical supplies, devices, pharmaceuticals and services on patient outcomes and reimbursement.
- Determine if implemented strategies are effective and achieving expected outcomes, clinically and/or financially.
External monitoring requires contract audits and service line experts to help you: - Track pricing and monitor supplier behavior.
- Stay up-to-date on the latest technological developments, perform ad hoc new technology assessments and report back to the value analysis team.
“When your value analysis program is mature, your organization should be examining spend data in the context of best practices, clinical outcomes and patient experience,” Alberto says. “Having the right tools to monitor your progress can make or break your success.”
HealthTrust Can Help
HealthTrust’s inSight Advisors—who are highly experienced in supply chain, clinical, workforce, IT, revenue cycle and various other health system functions—have developed analytical and tracking tools that support the value analysis process. With access to a proprietary database of more than 1,000 demonstrated best practices, HealthTrust can help hospitals establish a robust value analysis process or add rigor to an existing program. Methodologies focus on engaging physicians and key stakeholders to equip them with an effective, repeatable and sustainable means to stay ahead of continuous cost and quality pressures.
Learn more by contacting Vicki Alberto, vice president of clinical resource management, at victoria.alberto@healthtrustpg.com.
Share Email Finance, Performance Improvement, Q3 2018





