Two teams demonstrate the ripple effects of innovation
There’s no such thing as too many great ideas. That’s why, for the first time ever, HealthTrust has awarded two Innovation Grants to members with impressive initiatives for advancing healthcare performance. During the HealthTrust University Conference in mid-August, Boston Medical Center (BMC) and Centura Health were recognized.
As recipients of 2019 grants, both teams will receive $25,000 in cash and $25,000 in the form of consulting support from HealthTrust. Here’s a look at each team’s innovative plans and goals.
 Boston Medical Center
Boston Medical Center
High-performance operating room teams (HPTs)
It’s difficult to pinpoint the proportion of surgery-specific errors that contribute to the deaths of hospitalized patients each year. But with approximately 50 million operations performed annually in the U.S.—and medical complications believed to occur in up to 5 million of these cases—a group from BMC decided it was worth taking strong measures to cut the possibility of such outcomes.
At a national conference of the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) earlier this decade, a seed was firmly planted in the minds of attendees Pamela Rosenkranz, BSN, M.Ed, Director of Clinical Quality and Patient Safety in the Department of Surgery, and David McAneny, M.D., Vice Chair of the Department of Surgery. The idea was that the “best place to start if you want to reduce surgical complications is creating specialized teams,” Rosenkranz recalls. “We looked at each other and said, ‘Why don’t we have a dedicated OR team?’ ”
To start, Rosenkranz and McAneny aimed specifically at vascular surgery, based on data indicating that these patients experienced higher rates of surgical site infections compared to other surgical specialties. They approached Alik Farber, M.D., MBA, FACS, Chief of the Division of Vascular and Endovascular Surgery, who went all-in on the proposal.

Boston Medical Center
From left to right) David McAneny, M.D.
Donna Amado, RN, MSN Jeffrey Kalish, M.D.
Tracey Dechert, M.D.
Alik Farber, M.D.
Ingrid Rush, RN, MHA Katherine Scanlon, RN, MSN Pamela Rosenkranz, BSN, M.Ed
“We felt there was a lot of promise to not only improve operations but also clinical and social outcomes,” Dr. Farber says.
In 2015, the hospital launched its dedicated HPT in the OR for the vascular surgery service, including nurses, vascular surgeons, OR technologists, a service line coordinator, a nurse manager, an anesthesiologist and a quality improvement coordinator/facilitator. Robust data strongly supported the pilot initiative, indicating dedicated OR teams could reduce the likelihood of errors and postoperative complications.
Team goals were many, including developing positive working relationships, creating a culture conducive to sharing and analyzing experiences, improving process efficiency, enhancing patient and staff satisfaction and, ultimately, improving patient outcomes. Every other week, team members met—some coming in on their days off—to standardize OR procedures, such as patient preparation, by diagramming every major vascular operation. They would then gather in the hospital’s simulation lab to practice each newly refined approach.
Communication as a bedrock of success
Disrupted communication has proven to be hazardous for unintended surgical events, including retained instruments in the patient, wrong side/wrong site operations or procedures, and other adverse events.
A 2016 report found that communication breakdowns were responsible for 26% of malpractice claims related to surgery. As a result, one of the BMC’s team goals was optimizing communication by building open, transparent relationships. At the first meeting, everyone introduced themselves by their first name and last name only and revealed something about themselves outside the hospital that others might not have known.
“Everyone was on equal ground and got to know each other on a very personal level. It was amazing,” Rosenkranz says. “You could just see how the dynamics of that group changed.”
The team then took a mock patient from the OR’s holding area through the entire surgical process, analyzing each person’s role in the work stream. “It was amazing how many areas we uncovered from doing that exercise that needed work,” Rosenkranz says. “A lot of staff were leaving to get equipment they didn’t have, and the surgeons didn’t always have the right instruments. So we came up with a standardized major kit, minor kit and vascular cart.”
“Everyone was invested and energetic, and everyone had a voice,” she adds. “When we were in the operating room, what a difference that made in terms of improved personal interactions.”
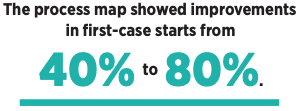
Farber also helped set up a process map to ensure thatsurgeries would begin on time. Its success led BMC to adopt the approach for all of its ORs.
Tangible results
The team’s overall impact was quickly tangible, with the Vascular Surgery HPT pilot leading to standardization of OR kits/preference carts and preoperative skin preparation along with intraoperative communication. Additional results included a decrease in OR traffic, the creation of a process map for first starts and a decrease in disruptive behavior.
Teamwork also led to a reduction in surgical site infections after leg bypass operations with the American College of Surgeons NSQIP data Odds Ratio improving from the 10th decile (1.75) to the 3rd decile (0.89).
“It’s a huge change and an objective improvement in a clinical outcome that I relate directly to the team and the way it worked together,” Dr. Farber says.
“Everything we did also had an impact on efficiency and staff satisfaction, which enhanced patient satisfaction,” Rosenkranz adds. “It was a win-win situation.”
Ripple effects
With the help of the HealthTrust Innovation Grant, BMC hopes the success of the pilot Vascular Surgery HPT will spread to other surgical specialties within the organization, with the intention to reduce errors and costs while improving patient outcomes. Three additional HPTs will be formed over the coming year, with the first incorporating vascular with cardiac, thoracic and transplant surgeries. The second team will include trauma, acute care and pediatric surgeries, while the third will cover minimally invasive, bariatric, colorectal and oncological surgeries.
The ultimate goal is for these efforts to ripple out to eventually include several other departments and specialties. Six domains have been defined to objectively measure gains from the new HPTs, including operational efficiency, quality, cost, staff and patient satisfaction, as well as relational coordination, a validated tool that measures teamwork across multiple industries, including healthcare.
The success of the HPT initiative can also be attributed to the backing it received from BMC’s executive leadership team and OR executive committee, Rosenkranz says.
“They are 100% supportive of this, because the goal is to create a culture of safety,” she says. “We feel if we have that, staff will want to come to work and do the best job they can. We want people to love what they do and like the people they work with. Staff satisfaction goes hand-in-hand with patient satisfaction.”
 Centura Health
Centura Health
Pharmacy referrals to digital care center
Clinical pharmacists are an important part of an interdisciplinary healthcare team. They provide expertise on safe medication use, including dosing, drug interactions, side effects and optimizing drug therapy. Due to the expansion of the Centura Health Provider Group, it was not possible to physically place a pharmacist at each clinic. To keep up with these challenges, Centura launched a digital care center, so patients visiting clinics could join a videoconference with a pharmacist.
Expanding the service within the first two years to more than 20 clinics and seeing a nearly four-fold monthly increase in patients served, Centura must keep up with the demand to serve its patients. The health system will use its HealthTrust Innovation Grant to help fuel the creation of a pharmacy referral process to the digital care center within the electronic health record.

Centura Health
(From left to right) Clint Hinman, PharmD, MPH
Lindi Lewis, PharmD, BCACP
Julie Prince, PharmD, BCPS
Driven by team members Clint Hinman, PharmD, MPH, Vice President of Pharmacy; Lindi Lewis, PharmD, BCACP, Telehealth Pharmacist Lead; and Julie Prince, PharmD, BCPS, Corporate Clinical Pharmacy Manager, the move will allow providers to refer any patient they feel would benefit from videoconferencing with a pharmacist while simultaneously lowering the burden on clinic office staff.
Ultimately, the end game is to enable the pharmacist to complete comprehensive medication management while using approved collaborative drug therapy management protocols for established disease states. The process complements the care provided by a patient’s primary care provider.
“This is an easier way for doctors to identify patients who need help from pharmacy. For example, by moving to comprehensive medication manage-ment, we can help to manage some-one’s diabetes or hypertension by using approved protocols,” Lewis says.
Expansion prompts service launch
Knowing how far Centura has come to reach this point requires a look back at where team members began. Several years ago, the idea of a remote pharmacist videoconferencing with patients visiting their primary care doctors for wellness checkups or after hospital discharge increasingly began to make sense.
At-risk patients with various disease states, such as chronic kidney disease or heart failure, began to be identified through a risk-stratifying scoring tool built into the electronic health record system that identifies patients most likely to benefit from ambulatory pharmacist intervention and scheduled for an upcoming visit with their provider. A list of eligible patients is sent to their primary provider, and those patients are contacted and asked to come in 30 minutes early and set up on an iPad to videoconference with the pharmacist located remotely at the digital care center.
During this conversation, the pharmacist performs an in-depth medication review with the patient, identifying medication issues along with missing lab tests and vaccinations. Recommendations are then sent to the patient’s PCP through a documented note in the electronic health record before the provider enters the patient’s room and conducts the medical visit.
“These patients need additional oversight with their meds and next steps,” explains Lewis, who conducts the remote assessments. “I’m looking at meds to see if they’re appropriate, making sure they’re dosed correctly and that there are no adverse reactions. I also ask the patient about side effects or check on compliance, to see if perhaps they’re not taking their medication because of cost or another issue.”
Impressive response
Centura has seen a continuous increase in volume since implementing the digital care center. The center served an average of 6.5 patients per month in its first year, with the average nearly doubling in 2018.
The center is currently serving 24.9 patients per month. While 93% of patients had never used videoconferencing with a healthcare provider prior to Centura’s digital care center, once a videoconference with a pharmacist was scheduled, 87% of patients completed those visits.
Survey results have shown a positive impact even with 85% of patients feeling overall knowledge of their medications prior to the visit was good, very good or excellent. When asked if they’d likely schedule or request a future virtual conference with a pharmacist, more than half (69%) responded with yes.
Physicians, too, have been supportive and enthusiastic because the program decreased the amount of time they need to review and counsel patients regarding medication management. For many, exposure to the virtual pharmacy was the first step into telehealth. One participating physician reports, “Virtual pharmacy just makes sense and could easily be a quickly expanding platform.” More than 80% of physicians responding to a survey found pharmacist recommendations to be helpful and 60% stated they were very helpful.
Refining and tracking results
Still, team members are clear-eyed about problems in the virtual pharmacy’s current model. In clinics, the burden of contacting patients to schedule a pharmacist videoconference falls mainly on medical assistants and patient service representatives. But some locations simply don’t have the capacity to add scheduling to these staff members’ existing workloads, limiting the number of patients who can benefit from the service.
As the sole pharmacist in the program, Lewis has also been swamped, currently receiving help from four pharmacy residents. “But we have another pharmacist starting,” Prince notes, “so we’re hoping we can reach more patients.”
With the help of the Innovation Grant, Centura plans to address those shortcomings by enabling physicians to refer patients they feel might benefit from virtual pharmacy visits while also reducing office staff workload. The grant’s service line component will lend consulting services to the effort, particularly in technology, lean process, project management, data mining, report development, and training and mentorship.
Existing metrics tracking pharmacy telehealth visits will be augmented by monitoring the number of patient referrals made by physicians to pharmacy each quarter, with the goal of continual growth. Additionally, the number of patients being assisted through a collaborative drug therapy management protocol will be tracked, and patient and provider satisfaction will be monitored through surveys.
“I’d like to see continued growth in the number of patients on comprehensive drug therapy management, so we can get to a larger population where we can track good quality outcomes. The ultimate goal is positively impacting patients and their overall quality of life,” Hinman adds.
Share Email Innovation Grant, Q4 2019





