Risk assessment tools across the continuum of care can help improve patient outcomes
Imagine a world where you could predict the future and know about all of your health issues before they happen. While we’re not there yet, healthcare professionals can now use predictive analytics, an area of statistics that provides the power to assess risk across various care settings. If used correctly, this analysis can help predict whether a patient will experience an adverse event before it occurs.

Michelle Smith, PharmD, FACHE, is Hospital Sisters Health System’s (HSHS) Chief Performance Improvement Officer for Information Technology. The health system uses tools to inform protocols. “We use risk assessments to look at how local system policies and procedures can be evaluated for common cause variation, share best practices and develop system standards that can be measured for actionable improvement,” she says.
Here are some of the options in today’s risk assessment toolkit, and what to keep in mind for the best results.
Pre-surgery or pre-procedure risk assessments
Procedure-related assessments, such as the Society of Thoracic Surgeons (STS) Online Risk Calculator, are used to identify a patient’s risk of developing complications. A score is calculated for many of the potential risks, including renal failure, stroke, prolonged ventilation, length of stay, infection, re-operation and mortality. This enables more- informed conversations among providers, patients and their families in shared decision-making, as well as improved preparation of the surgeon and staff.

Karen Bush, MSN, FNP, BC, NCRP, Director of Clinical Research & Education at HealthTrust, says to keep in mind that obtaining the score is only part of the puzzle. Using the score to appropriately treat the patient requires a directed team approach and a physician who is engaged in the process. “The drawback of this type of system is that typically the information used for these risk assessments must be manually entered into a proprietary system to obtain a score. Often, these are not integrated into the hospital or physician office’s electronic medical record,” she adds.
In July 2019, the American College of Surgeons launched a new geriatric assessment tool
called the Geriatric Surgery Verification (GSV) Program. Recognizing that the population is rapidly aging and has specific needs, the group created a program that addresses 30 standards of surgical care for older adults. The benefits include better patient-physician communication about the patient’s goals, as well as higher-quality, lower-cost surgical care.
Warning score systems
Early Warning Scoring (EWS) systems are used to detect the risk of potential adverse events
while a patient is in the hospital. Assessments such as the Modified Early Warning Scoring (MEWS) use physiologic data points in the medical record to create an early warning system to notify hospital staff that a patient’s condition is worsening, as well as the severity of the situation.
Smith shares that one of her organization’s ongoing priorities is fall prevention. “At HSHS, we use the Hendricks Fall Risk Assessment, which we have built into our screenings,” says Smith. The HSHS process is to escalate a patient’s fall risk potential based on algorithms. If clinicians see an uptick of falls in a certain area, they can use the assessments to create a plan of action for improvement.
“We are looking at the number and types of falls to categorize them,” says Smith. This information allows the team to better determine where to focus their efforts. “Falls can really be a setback for our patients as they try to heal. They can lead to a longer hospital stay and higher bills. We want to make sure we aren’t adding to the cost of care, and that is why we are looking at how to prevent falls in a sustainable way based on the patient population.”
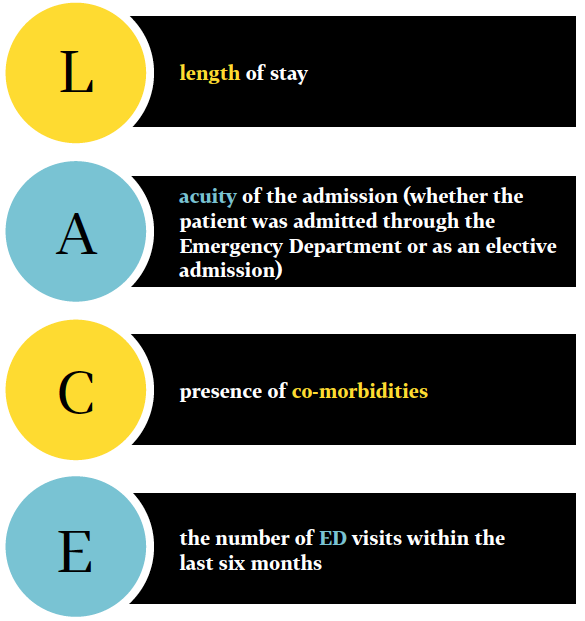
Evaluating patients’ vulnerabilities as they transition from hospital to home offers healthcare staff the ability to identify risk and provide additional resources to avoid adverse events. The LACE Risk Assessment is used to evaluate a patient’s risk of death or readmission after discharge from the hospital and to drive interventions for patients, based on the patient’s score. The score is calculated using the four categories shown in the following graphic.
For example, heart failure patients who are identified as high risk for readmission on a LACE score may have a transition coach assigned to their case with additional education or tools employed while in the hospital. They may also receive more frequent touchpoints via phone or in person after hospital discharge, follow-up appointments made with the patient’s regular physicians within a week of discharge, and additional resources such as home healthcare or cardiac rehabilitation.
No matter which tools facilities employ for the prevention of adverse outcomes, they should be easy to use and effective at identifying risk, Bush points out. Most important, risk assessment tools must be used to influence patient care to reduce that risk. “A tool that is used to calculate risk without specific protocol as to who should do what with the results is like having a car with no gas. It doesn’t go anywhere,” she says.
For more information on risk assessment tools, contact Kimberly Wright, RN, AVP of Clinical Data Solutions.
Share Email Q1 2020





