7 ways to foster physician engagement with supply chain decision-makers to bolster value analysis
Value analysis initiatives can help hospitals and health systems improve patient care while reducing supply costs. Engaging physicians in this process, securing their buy-in and benefiting from their clinical expertise is crucial to a successful value analysis program.

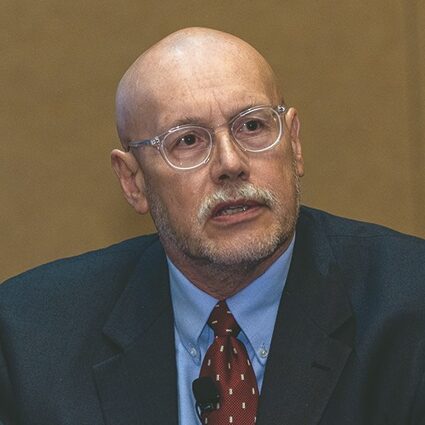
However, supply chain leaders often struggle with formally involving physicians in value analysis processes and programs. At the 2023 HealthTrust University Conference, three HealthTrust Physician Advisors joined HealthTrust’s Chief Medical Officer, John Young, M.D., MBA, FACHE, to discuss best practices for engaging physicians in value analysis in a panel discussion titled, Bridging the Divide. “I’ve been doing this for about 25 years, and I don’t think there’s ever been a time when the financial and the business piece have dominated the conversation equal to the clinical piece,” Dr. Young said. “And that’s what we’re trying to bridge.”
Their discussion led to seven key principles teams can follow when closing the gap between supply chain and clinicians.
1. Begin with low-hanging fruit.
To ease physicians into the value analysis process, identify opportunities for change in areas that are integral to their day-to-day work, but simple to adapt to.
Bert Altmanshofer, DPM, a podiatric medicine specialist practicing in Duncansville, Pennsylvania, said it starts with laying the foundational groundwork, just like you would at home. “What do I tell my family? First, we can shut off the lights when we’re not using them. We can fix the leaky faucets. These are easy things we can do, so those were the basics that we started with,” he said.
Beginning with the fundamentals at his facility led to more widespread change. “We then developed strategies and lists of wants and needs. As subspecialty groups, we had to start looking at the wants-versus-needs list and grow from there,” he added. “For us, that was huge. It got everybody involved, making sure everybody expressed an opinion.”
2. Use data to win physicians over.
Dr. Young recommended being direct and transparent while leveraging data and evidence to engage physicians. This is the approach that HealthTrust takes when its Advisory Services team works with members on value analysis engagements. “With benchmarking and utilization data we can show them that their cost per case is high compared to everyone else’s,” he said. “You can then gently but collegially use peer pressure to drive those outliers down. No one wants to be the most expensive doc per case in the hospital.”

Elise Denneny, M.D., FACS, an otolaryngologist practicing in Knoxville, Tennessee, said physicians are universally driven by the core value of wanting what’s best for patients, backed by science. “Physicians are data-driven. If you present the data and the logic, for the most part, you can win them over,” she said. “One physician on our staff wants things done in the next 24 hours. Everybody attributes it to ego, but what’s driving that ego is a belief in providing the best patient care. When we got him to look at the data on how this impacts the entire healthcare system, we were able to bring him around.”
Dr. Altmanshofer explained how the data piece has been a game-changer for his organization: “Suddenly, there were reports. There were expectations. We set goals and explained how we were going to achieve them,” he said. “We were able to say, ‘Listen, if we meet these marks, we’re going to be able to add employees, we’re going to cut down on the call schedule for our nurses in the OR, we’re going to be able to shift people around a little bit.’ ”
3. Establish shared decision-making.
Instead of using a top-down approach, create structures, processes and accountability around shared decision-making that allows physicians to affect change and have their voices heard. “Physicians want three things. They want autonomy. They want respect. They want to be heard,” said Dr. Denneny.

“When you’re talking with colleagues about something concrete, like choosing one particular implant over another, it can be an extremely difficult conversation,” said Aron Wahrman, M.D., MBA, a plastic surgeon at the Perelman Center for Advanced Medicine in Philadelphia. “But as long as they feel their opinion is valued and they have a voice, you can work through these difficult conversations—even if the choice may not be the one they ultimately wanted. You can suggest that down the road, when we examine the outcomes data, if we are not doing as well with this choice of implant, then we’ll re-examine.”
4. Take action.
Physicians need to see that their involvement in the value analysis process leads to tangible outcomes at every step. “We learned that one of the worst things you can do is engage physicians, have them do a bunch of data analysis and sit through multiple meetings, only to have nothing happen. There has to be action because, otherwise, you’ll lose them,” said Dr. Young.
Dr. Denneny also stressed the importance of progress. “I like seeing three actionable items at the end [of every meeting]. So we’ve not wasted your time, but respected your time,” she said.
Ongoing action can be motivation to remain engaged, explained Dr. Young. “One of the reasons members re-engage our teams is because value analysis is a continuous process. New products, technology and pharmaceuticals come along frequently, so you change, adapt and modify,” he said. “We work to show these value analysis teams that it’s not a rigid structure. It’s an opportunity to open another door.”
5. Establish alignment on shared goals and culture, rooted in trust.
Agree to a common mission and vision for the value analysis process, which should also align with the overall goals of the organization. Clinicians are more likely to participate when patient outcomes and quality of care are at the forefront of the process.
“A shared mission and culture of trust comes from the top down, with confidentiality built in. If you disagree with your team member, you don’t go tell everyone. It doesn’t serve anything, other than to reflect poorly on you,” Dr. Denneny said.
“We saw a change in our facility around the culture of safety. We require our value analysis team members to go on patient safety rounds once a quarter,” Dr. Altmanshofer explained. “From that we helped to spread this culture and value and started to understand the integration: Why do you do this in the unit? Why do you do this on the dock? As we looked at those things, we realized how well all of the pieces fit together.”
6. Bring together a collaborative multidisciplinary team, including a physician champion.
Value analysis teams should include all the relevant stakeholders, including physician and nursing leaders, service line heads, IT support and, ideally, a member of the executive team.
Dr. Wahrman recommended taking advantage of the expertise and first-hand experience of clinicians. “You want people who are familiar with a particular device. We get a sense from our own use and what’s in the literature as to what is on the horizon, and what may be comparable but potentially more cost efficient,” he added.
Finding your physician champions to build support and influence change is also crucial. “You can be a brilliant clinician, but it doesn’t necessarily mean you’re going to be good at collaborating, building teams or having these kinds of conversations,” explained Dr. Young. “You have to find people who are interested, share the vision and who will roll up their sleeves and get to work.”
7. Standardize your definitions.
In healthcare, the value equation—value equals outcome divided by cost—is far from a simple math problem, Dr. Wahrman said. Cost can be easily measured, but questions abound around how to attach numbers to value and outcomes.
“If a cardiologist performs a stent procedure, how do you measure the outcome? Is it by how many more years a patient had or by how many more ‘good’ years they had?” asked Dr. Wahrman. “Many things go in to measuring value and outcome, but it’s far from being standardized.”
That’s where a strong value analysis program comes in. HealthTrust has developed analytical and tracking tools that support the value analysis process. With access to a proprietary database of more than 1,000 demonstrated best practices, HealthTrust’s Advisory Services team can assist your organization in establishing a robust value analysis process or enhancing an existing program. Methodologies focus on engaging physicians and key stakeholders to equip them with a repeatable and sustainable process to stay ahead of cost and quality pressures.
Increase the effectiveness of your value analysis program with best practices from HealthTrust Advisory Services.
For more information, contact your HealthTrust Account Manager or visit Value Analysis.
Share Email Physician Advisor, Q1 2024